|
CUTANEOUS STRUCTURE
|
|
|
In the earliest days of fetal life, the epidermis is a single sheet of cells, which is doubled between the fifth and sixth week .The outer layer, is the periderm and the inner layer is the stratum germanitivum. The stratum germinatum is responsible for the development of most epithelial structures of the skin such as the basal cell layer, and eccrine sweat glands. The primary epithelial germ cells give rise to the sebaceous glands, apocrine glands and hair follicles. Stratum Malpighi appears in the four months of fetal life.
STRUCTURE OF INFANT SKIN The dermoepidermal adhesion in babies is less than in adults. This explains the stronger skin reactions in infants and young children in response to certain stimuli such as in bullous papular urticaria due to insect bites or other stimuli. The heat regulation mechanism in infants differs than in adult skin. The differences are mainly due to variations in area-to-body volume, ratio of skin vascular reactivity and the tendency of loosing heat by sweating where, all of these can lead to more loss of heat in infants after minor stimuli.
PHYSIOLOLOGICAL CHANGES
OF NEONATAL SKIN AND ITS APPENDAGES At birth the skin is covered with a whitish greasy film, which is the vernix caseosa. The vernix may cover the entire skin surface or it may be present only in body folds such as the groins. It normally dries rapidly and starts to flake off within a few hours after birth. Different color changes may appear in the newborn. Golden yellow staining occurs in hemolytic diseases of the newborn and post maturity. Bile pigments staining of the vernix and muconium occurs in fetal distress. Vivid color difference may appear along the midline at some time during the first week of life. This phenomenon occurs when the baby is lying on its side, the upper half of the body becomes pale while the lower half has a deep red color with a sharp midline demarcation between the two. Peripheral cyanosis (or acrocyanosis) is a feature particularly seen in the full term newborn. Generalized hyperemia is usually known as erythema neonatorum, which fades spontaneously within few days. Scaling of the skin of the newborn occurs in most normal neonates. Superficial cutaneous desquamation is often physiological. One or two solitary blisters or erosions are occasionally present at birth on the fingers, lips or forearms. These are due to vigorous sucking in utero; hence the term sucking blister is often applied. Sebaceous glands hyperplasia is usually considered a physiological event in the newborn, reflecting the influence of maternal androgens. Multiple, uniform, pinpoint yellowish papules appear mainly on the nose, cheeks, upper lip forehead, genitalia and the limbs. The lesion usually clears spontaneously without treatment Sweat ducts - papules may appear on the face and genitalia due to temporary obstruction of the sweat ducts, which usually disappear during the first weeks of life. These changes are related to maternal and placental hormones. Hair - lanugo hair covers the skin of the newborn that may be pigmented. This usually sheds within few weeks. The Female Genitalia - a mucoid vaginal discharge is common in the female newborn. Vaginal epithelium desquamates to leave a more normal infantile mucosa , this desquamation may be accompanied by a creamy white discharge. Frank withdrawal bleeding may occur from the uterus on the third or fourth day, usually lasting 2 - 3 days. The male genitalia appear similarly large and well developed at birth. Breast
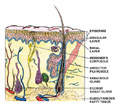
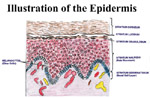
EPIDERMIS The different layers of the epidermis include the stratum corneum, stratum granulosum, stratum malpighii (prickle cell layer), stratum spinosum, (ret mucosum) and the basal layer (stratum germinativum). In palmoplantar skin there is an additional zone, the stratum lucidum between the stratum granulosum and the stratum corneum.
Stratum Granulosum (granular layer) - lies on the top of the prickle cells and consists of rows of flattened nucleated cells, which contain keratohyaline granules. Stratum Malpighi (prickle cell layer) - lies on the top of the basal layer and following its direction. This is a very important layer and is involved in most of the pathological conditions of the skin. Stratum Germinativum (Basal Layer) - is the deeper layer of the epidermis and is composed of a single row of columnar cells arranged vertically to the basement membrane. The cells of the basal layer become modified to form all other cells of the epidermis. The epidermis is maintained by the division of the germinate cells present in the basal layer and differentiate later to keratinocytes in about seven weeks.
Epidermal cells are composed of keratinocytes, melanocytes,mast , Langerhans cells and undefined cells.
As the keratinocytes move upwards reaching the granular layer of the epidermis, loose their nuclei. Keratinocytes become flattened and heaped on the skin surface as horny dead cells. The thickness of this layer varies according to age and different body sites. Vitamin A is found to have an important role in the development of keratinocytes. Fetal epidermis, with incomplete keratinization, has abundant glycogen, which is present in the outer root sheath of active hair follicles. Glycogen is found to increase after epidermal injury, which has a direct relation to cellular metabolism. Keratinocytes possess A and B blood group antigens and share with the red blood cells the same antibodies that are absorbed selectively in some immune reactions. Functions of keratinocytes
DERMIS
(corium) The entire surface of the dermis is beset with numerous papillae which are more numerous in some locations such as areola of the nipple and terminal phalanges. Most inflammatory diseases of the skin involve the papillary dermis. The deeper part of the dermis is the reticular layer, where injury below that level leads to scarring after healing. The dermis contains and supports blood vessels, lymph vessels, nerves, hair follicles, glands and muscle elements.
The cells of the dermis are derived from the reticulum cell, the primitive mesenchymal cell. The cells of the dermis include :
The dermis is composed of:
The dermis contains the specialized sensory organs and the skin appendages. Below the dermis is a fatty layer known as the subcutaneous tissue.
The dermis has a very rich blood supply, though no vessels pass the dermoepidermal junction.
Cutaneous enervation depends upon dermal nerve network, which has special sensory nerve endings. The motor innervation of the skin is autonomic. This includes a cholinergic component to the eccrine sweat glands and adrenergic components to both the eccrine, apocrine glands, to the smooth muscle, the blood vessels and to the erector pilorum muscles. The sensory nerve endings are of several kinds: some are free, some terminate in the hair follicles and others have expanded tips. The special sensory nerve endings in the dermis are of several different types mainly, the Vater-Pacini corpuscles and the Meissner corpuscles. Merkel‘s corpuscles are found on the sides of the tongue. Krause‘s corpuscles are found on the conjuctiva while Ruffins corpuscles are present on the soles.
Hair is present on all parts
of the human skin except the palms, soles, red portions of the lips,
ungual phalanges and glans penis.
The outer root sheath extends from the epidermis to the hair bulb.
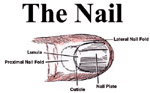
The nails are convex, translucent horny plates that are composed of:
|
|||||||||||
| Contents | Index of photos | Next Chapter >> | Search |