|
OTHER TYPES OF DERMATITIS
|
|
|
|
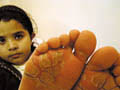
Microorganisms or their products that clear when the organisms are eradicated may cause microbial eczema. This should be distinguished from infected eczema, in which eczema is complicated by secondary bacterial or viral invasion of the broken skin. The skin becomes sensitized to bacterial products or chemicals present in the exudates. Infectious eczematoid dermatitis is considered as an example of autosensitisation. The mechanism by which microorganisms can cause eczema is not understood. Bacterial antigens can promote a cytotoxic reaction in the skin. Clinical Features The distinction between infective and infected eczema is difficult. Infected eczema shows erythema with exudation and crusting. The exudation may be profuse with crusting, or slight, with the accumulation of layers of somewhat greasy moist scale, below the surface is raw and red. The margin is characteristically sharply defined. There may be small pustules and fissures in the advancing edge . Infective eczema usually presents as an area of advancing erythema, sometimes with micro vesicles. It is seen predominantly around discharging wounds or ulcers, or moist skin lesions of other types. Infective dermatitis is relatively common in patients with venous leg ulcers, but care must be taken to distinguish it from contact dermatitis due to topical preparations . Staphylococci or streptococci can be cultured and the lesions respond to antiseptic and antibiotic therapy . This condition seems to occur particularly in patients with poor standards of hygiene. Hyperhidrosis and heavy footwear may be an important predisposing factor . Infective dermatitis may also complicate chronic threadworm infestation, pediculosis, scabies and excoriations of the skin due to repeated scratching . Plantar eczema in children ,this must be distinguished from juvenile plantar dermatosis. Tinea pedis may also become eczematous due to the overgrowth of Gram-negative organisms . Treatment
NUMMULAR
DERMATITIS Nummular dermatitis is a chronic eczematous lesion that is caused by different known and unknown factors. The condition may be preceded by atopic dermatitis. The lesion may appear as a separate entity as annular, coin-like or discoid lesions on the extensor surface of the extremities, trunk and the buttocks . This type of eczema appears mainly in older age groups . Predisposing Factors Insect bites : the papular and urticarial lesions may become chronic in neglected untreated cases or by the repeated severe itching and excoriation. Late manifestation of atopic dermatitis :Discoid eczema may appear at the end stage of chronic atopic eczema Irritating agents : irritants whether external such as topical sensitizing creams, detergents, metal or internal allergens may cause nummular dermatitis. Dryness of the skin: dryness of skin due to different factors such as excessive bathing , using harsh and medicated strong alkaline soaps. In older age groups the skin usually tends to be drier. Psychosomatic disorders may be considered an important predisposing factor. Autosensitisation. Drug reaction. Drug reaction due to different drugs such as sulfonamides and methyldopa, where the fixed drug lesion may appear on the previous eczematized site . Clinical Features Acute type Skin lesions are annular or coin-shaped papulo vesicular patches or plaques on an erythematous base. Oozing surface of the lesion may occur with excessive excoriation due to itching or rubbing followed by secondary bacterial infection. One of the characteristic features of nummular dermatitis is that the patches that seem to be dormant may become active again, particularly if treatment is discontinued. Chronic type Atopic dermatitis in childhood is liable to become discoid eczema later on. Cases of chronic discoid eczema have usually an atopic history. In the chronic stage , the lesions are dry and excoriated coin shaped. These are single or multiple lesions and may be accompanied by severe itching which usually increases with different irritating factors such as emotional stress. Secondary lesions may follow later on involving the limbs or the trunk. Fig.211a. Discoid eczema The course of this type of eczema is very chronic and has the characteristic of relapse and remission, where after healing of the lesions, new recurrent eruption occurs at the same older site . Treatment Elimination of the irritating factor if possible . Mild topical steroid alone or combined with an antibiotic or salicylic acid (Locosalene, diprosalic, salidecoderm) in an ointment base especially in dry lesions . Antihistamine preparation such as Citrizine is given for few days preferably at bedtime, where itching is more severe at night and to combat the possibility of sedation especially with old sedating antihistamines. Corticosteroids orally or parentally are rarely indicated in nummular eczema.
DYSHIDROTIC
ECZEMA Dyshidrotic eczema is a deep vesicular skin reaction involving the fingers, the interdigital spaces and the feet. The vesicles have a characteristic morphological appearance as that of sago grains. The condition is rare in young age groups and more common in adults . Predisposing Factors
The lesions are vesicular and usually symmetrical accompanied with mild or severe itching. Excoriation of the lesions is not uncommon.
The vesicles of dyshidrotic eczema involute spontaneously and do not rupture as in other vesicular skin lesions. Treatment
JUVENILE
PLANTAR DERMATOSES Juvenile dermatoses affects mainly children . Both feet may be involved symmetrically and become macerated. Predisposing Factors Sweat retention and occlusion of the feet by woolen or polyester socks. Keeping the foot for a long time without aeration is an important triggering factor.
Clinical Features Both soles are involved which become macerated and fissured. The interdigital spaces and the weight bearing areas are spared . Treatment
The skin manifestation is characteristically on the inner lower leg above the internal maleolus. The lesion appears as a cyanotic , erythematous and edematous due to local congestion. The condition may be accompanied by mild itching, lichenifecation, ulceration and hyperpigmentation.
|
| Contents | << Previous Chapter | Next Chapter >> | Search |