|
FUNGAL
SKIN INFECTIONS
|
|
|
|
TINEA CAPITIS T. Capitis is a worldwide problem fungal infection of the scalp. It is primarily a disease in young children where, males are more infected than females. This may be due to shortness of the hair, which facilitates easy reach of the fungal spores to the scalp. Adults are rarely infected; this is believed to be due to the higher fatty acid of the scalp, which have dermatophytes inhibiting property. It was established many years ago that some saturated fatty acids, from adult human hair (and derived from sebum) were inhibitory to dermatophytes fungi. Fungal scalp infection may be endemic, sporadic or epidemic, where involvement of large number of school children or in crowded low hygiene refugee camps is not uncommon. The tendency of scalp ringworm to clear spontaneously at puberty was believed to be due to the change in sebum composition at this age. T. Capitis infections are common in temperate countries. Contact with infected persons or their fomites such as combs, brushes, or headgears. Contact with infected pets or animals such as cats, dogs or cattle. Minor trauma is an important predisposing factor for seeding of the fungi on the scalp to cause infection. Curiously, human-to-human infection of M. canes infections seems to be low and once treatment is established children can go back to school. Different Fungal strains causing infection Microsporon auduini - is the most common strain to cause T. Capitis. Microsporon canis - is often contracted from animals, can cause highly inflammatory lesions. Trichophyton mentagrophyte - causes highly inflammatory T. Capitis. Tricophyton Tonsurans - causes an exceedingly chronic infection. The fungal infections often are familial. T. Violaceum - causes the clinical lesion called "black dot" ring worm T. Schoenleini - causes the clinical type of T. Capitis known as favus. Clinical Features The clinical picture usually varies according to the causative dermatophyte. Some strains such as Microsporon Canis and T. Mentagrophtes cause highly inflammatory lesions, while T. Tonsurans lesions have a very chronic course. The clinical picture may be sometimes confusing and cannot be easily diagnosed except by detection of the dermatophyte by potassium hydroxide smears. Different clinical types of Tinea Capitis:
Diagnosis Diagnosis of T. capitis can be settled by different methods:
Technique: Collection of scrapings from the infected skin should be taken from the active edge of the lesion using a blunt scalpel blade or by the edge of a slide. Infected hairs should be depilated from their roots especially in favus. The specimen is placed on a slide and a drop of 30 percent potassium hydroxide is added and covered by a cover slip . This is heated gently in order to soften and clear the material . Care should be taken in order not to heat the specimen too much and not to boil . The specimen is examined with low power microscope without staining. This may show the branched septate hyphae. Hair invasion by dermatophyte is ectothrex in Microsporon, T. Mmentagrophyte and T. Verrucosum, while it is endothrix in T. Tonsurans and T. Violaceum.
Differential Diagnosis
Treatment Preventive measures Topical treatment Systemic treatment
Mode of action: The mode of action of griseofulvin appears to be in part by inhibition of formation of microtubules and it is most apparent in the active metabolizing cells near the hyphal tip. In man, griseofulvin is fairly rapidly metabolized and conjugated with glucuronide in the liver, excreted by the kidney and by the liver in bile. Interaction Griseofulvin interacts with certain drugs such as anticoagulants, warfarin, cyclosporin , barbiturates and oral contraceptives. Dose: Griseofulvin is available in the standard microcrystalline form as 125 mg and 500 mg tablets and as a pediatric oral suspension, 125 mg per 5 ml given after meals preferably after a fatty meal , which increase drug absorption. In Tinea capitis a single dose, 2 g. of griseofulvin especially in young children (in order to be sure that the effective dose was given), is frequently enough to clear most of the lesions . The recommended daily dose is: A. Infants and children:
Special indications of Azoles Widespread Tinea corporis due to T. rubrum , azoles are the treatment of choice. Cases that failed to respond or cannot tolerate griseofulvin Type of azoles available Itraconazole - these are effective new anti-fungal preparations. Dose: Adult: 100-200mg. /day for few weeks in skin fungal infection and for several months in onychomycosis.. Side effects of itraconazole:
Side effects:
Interactions The drug interacts with the following:
Contra-indications Severe hepatocellular failure . Terfenadine or astemazole concurrent use . Pregnancy Breast-feeding Allergy to the drug .
5- Terbinafine: Terbinafine such as
Lamasil can be given orally. The adult dose is 250 mg daily. Terbinafine is available also as topical preparation (Lamasil cream). It has produced rapid and long-lasting remissions in both nail disease and persistent Tinea pedais. There is some evidence to suggest that the frequency of relapse is much lower with Terbinafine than that with other antifungal preparations. 6- Voriconazole: The anti-fungal agent voriconazole is well tolerated,
with only mild to moderate adverse effects, report researchers.
ONYCHOMYCOSIS Fungal infection of the nails has a chronic course , slow and may take few months to manifest . The severity and effect of infection of the nail is rather much dependent on the type of infecting dermatophyte . Different Fungi causing onychomycosis:
The nail plate remains hard and glossy as the normal nail in contrast to infections caused by dermatophyte, which lead to broken and friable, nails.
T. Corporis is an inflammatory mycosis of the glabrous skin. Different species as Trichophyton, Microsporon and Epidermophyton floccosum can cause the disease. Modes of Infection
The most common sites involved are the exposed areas such as face, neck and extremities especially in children, but any site of the body may be involved. Body ringworm lesions present with erythematous papules, which enlarge to the periphery. The fungus consumes the keratin at the center and retreats away from the primary inoculation site, forming an oval or circular plaque with elevated papulo-vesicular active edges more inflamed than the center. The lesions sometimes form inflamed circles alternating with pale scaly areas.
Course of Tinea Corporis: T. corporis lesion may heal spontaneously. May become a highly inflammatory lesion. May run a chronic course. Dissemination may spread to other parts of the body. Secondary bacterial infection may invade the area. Differential Diagnosis: Psoriasis Pityriasis rosea Parapsoriasis This is a fungal lesion of the skin that appears as a small papule, which enlarges eccentrically, where the dermatophyte consumes the keratin in the center and then moves to the periphery leaving scaly hypopigmented center and raised active edges. Fig. 71a. Tinea circinata (Vesiculo-bullous and crusted lesions on the active periphery with central clearing) Clinical Features Circinate lesions may fuse together forming large plaques or gyrate lesions. The symptoms are minimal apart from mild itching. The condition is mildly contagious. These lesions form different clinical varieties:
Crusted lesions covering wide areas of the skin and scalp with a mousy smell. The characteristics of this type are Scutula and heavily crusted lesions as that occurring in favus.
This is a boggy inflammation of the glabrous skin as that of the kerion, which occurs on the scalp. The condition is caused by dermatophytes transmitted from animals such as T. verrucosum. Clinical Features Different clinical types of Tinea profunda:
GRANULOMATOUS RINGWORM This is a rare form of follicular and perifollicular granulomatous ring worm which has a chronic course. Clinical Features The lesion appears on the glabrous skin mainly on the chins as a circular, raised, circumscribed boggy-crusted lesion in which the follicles are distended with a viscid purulent material.
This is a superficial fungal infection of the glabrous skin. The lesions present with extensive patches that appear as concentric rings with polycyclic borders and scaly edges. The course may take a long time where hyperpigmented and residual hypo-pigmentation appear after healing of the lesions.
Favus is a fungal infection of the scalp, caused by Trichophyton Schoenleini. Children are the main age group infected with favus. The infection rarely involves the glabrous skin as trunk and neck. The lesions may present with thick and crusted patches. Differential Diagnosis of T. Corporis
Tinea Corporis lesion has an active vesiculo-papular elevated edges while in pityriasis rosea the edges are smooth. Herald patch (which is a large erythematous plaque preceded the appearance of the skin eruption) may be detected. The distribution of pityriasis rosea lesions is usually along the line of ribs. When there is a problem in the differential diagnosis, potassium hydroxide smears can detect the causative fungal species in T corporis. Discoid Eczema - the lesion is more itchy, round erythematous, scaly and there is no elevated active edge such as in T. corporis and no fungal elements detected on microscopical examination. Discoid lupus erythematosus - The sites involved are mainly sun-exposed areas. No papulo vesicles appear on the edges. The lesion of discoid lupus erythematosus has adherent scales. Heals with scarring. Psoriasis - silvery scales covering the patches with no central clearing. Diagnosis
Treatment of T. Corporis Topical Preparations Mild solitary lesion: may need only topical antifungal preparation such as Tolnaftate or imidazole derivatives as Miconazole, Ecanozole nitrate, Clotrimazole and Chlormidazole. Localized tinea corporis, especially of recent origin, commonly responds usually to topical antifungal preparations, applied twice daily for about a month. Severe inflammatory fungal lesions: are treated by combination of oral and topical antifungal medications. Care should be taken in using topical steroids in fungal lesions. Topical steroids may suppress the inflammation and irritation, but it masks the clinical picture besides the side effect causing striae and skin atrophy especially the delicate skin of the intertriginous areas when used for a long time. Systemic Preparations Systemic treatment by griseofulvin or the other new generation antifungal drugs the Azole groups should be used in wide spread lesions, or cases not responding to topical preparations or in follicular lesions. In more widespread infections of recent onset, griseofulvin will generally be preferred and may be expected to clear the condition in about 4 weeks. Where the infection is long-standing, for example, when caused by T. rubrum, much longer-term intermittent courses for 3-4-weeks intervals, over a period of several months may be required. Ketoconazole appears to be less satisfactory than griseofulvin in Tinea imbricata, although preliminary data suggest that itraconazole may work better.
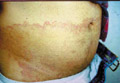
Tinea Cruris is a superficial fungal inflammation of the intertriginous areas mainly that of the inguinal, gluteal and the axillary areas. The most common dermatophytes that can cause T. cruris are Epidermophyton floccosum and Trichophyton rubrum. Severe inflammatory lesions are rare and are due to the species T. Mentagrophtes and T. Verrucosum. Tinea Cruris occurs mainly in adults but infants and young children are rarely infected. During the last twenty-five years I have seen a very few cases of Tinea cruris due to dermatophytes in infants and young children. Tinea cruris due to Candida are the most common fungal infections in infants and young children. Predisposing Factors Occlusion of the crural area such as by diapers or plastic pants. Excessive sweating and maceration. Modes of inection Infection may be contracted from infected domestic animals such as cats or dogs. Infected materials such as towels or others. Auto inoculation from fungal focus elsewhere. Epidemic infection in school children may occur especially when sharing training suits, swimming kits or infected clothes Clinical Picture The lesion may begin in the crural area on the side of one thigh and extends to the other side to become bilateral. Spread of the lesion may extend to the adjacent areas to the intergluteal cleft, groin and upper abdomen. Scrotum is usually not involved; this may be due to the thin musculature of the area and continuous movement of the scrotal muscles that may cause difficulty for the fungus to seed there. The lesions begin as an erythematous scaly area spreading to the periphery with an active elevated edge, where itching is a predominant feature. The lesions in the early stages are in the form of erythematous macules or plaques, arciform with sharp margins extending from the groin down to the thighs. Scaling is variable and occasionally may mask the inflammatory changes. Central clearance is usually incomplete with nodules scattered throughout the affected area. Satellite lesions if present are few in number and relatively large. The course of the lesion depends on the causative dermatophyte. The clinical picture usually varies according to the type of dermatophyte: Epidermophyton floccosum infections - are typically acute in onset, rather inflammatory and often primary. Trichophyton rubrum - lesions are usually chronic. Extension from the groins to other sites is common. T. Rubrum lesions extend to the buttocks, the lower back and the abdomen. T. interdigitale - infections may be vesicular and inflammatory.
Fig.76d. Erythrasma(For differential diagnosis) Fig. 76d. Tinea versicolor( For D.D.) Differential Diagnosis Seborrheic dermatitis - the lesion presents with diffuse erythematous patch free from central clearing and has no active edges such as the lesions of T. Cruris. Greasy scales cover the lesion in seborrheic dermatitis. No fungal elements are detected on microscopic examination. Pityriasis rosea: the lesions are oval or rounded discreet patches with few scales on the center. The edges are not raised and herald patch may be detected elsewhere. Erythrasma - the lesions covers the infected area without central clearing. No active edges as in T. Cruris. Erythrasma gives coral red color with Wood‘s light. Microscopic examination of the scraping of the lesion shows the causative bacteria. Candidiasis - Satellite lesions appear on the sides of the lesion.
T. pedis is a mycotic infection of interdigital spaces, sub-digital folds, the soles and other areas of the skin. Dermatophytes (T. Rubrum, T. Interdigitale and Epidermophyton floccosum), yeast and moulds are the causative fungi. The disease is more common in adult males and mainly in temperate zones.
Fig.77c. T. pedis ( due to Candida ) Fig.77c. T. pedis ( due to dermatophytes)
Epidemic cases of T. Pedis may occur especially in school children and other groups under certain conditions facilitating spread of fungal infection.
Clinical picture Maceration of the interdigital area between the third or fourth toe web space or beneath the interphalangeal crease of the last three toes accompanied by inflammation and vesiculation. The clinical picture usually depends on the type of the fungus causing the disease. T. Interdigitale causes the acute vesicular lesions predisposed by excessive maceration of the interdigital area. Vesicular eruption appears in the interdigital area with vesicles on an erythematous base containing clear yellow liquid. Secondary infection of the vesicles may cause more inflammation accompanied by itching and pain. T. Rubrum causes the chronic dry and scaly type of T. Pedis. The infection may spread to the adjacent tissue and nail causing onychomycosis. Treatment of Tinea Pedis
Tinea versicolor is a superficial fungal infection caused by Malassezia Furfur. The infection is most prevalent in the tropics predisposed by excessive sweating. T. Versicolor is unusual in children and young age. Infection occurs from using infected clothes, towels and bed sheets. Autoinfection is also common. Clinical Picture T. Versicolor has a chronic course and recurrence is common due to auto- infection or due to re-infection. Erythematous scaly macules and patches appear on the trunk shoulders, upper neck and upper limbs. Pityriasis versicolor is usually asymptomatic. The condition rarely forms a distinct problem except for cosmetic. Hyperpigmented patches intermingled with hypopigmented areas appear on the affected site. Pruritus is minimal but may increase with excessive sweating and bathing. The condition may have a chronic course extending months and even years recurring every summer if not properly treated.
Fig. 80b Tinea versicolor (Uncommon wide spread lesion) Fig. 80 Tinea versicolor Fig. 80b. Tinea versicolor ( chronic lesion misdiagnosed as vitilligo) Differential Diagnosis Tinea corporis - the lesion is more inflammatory with raised active edges and the dermatophytes can be detected microscopically. Vitilligo - the pigmentary loss in vitilligo is complete and the patches are white, smooth and without the branny scales. Tuberculoid leprosy - the clinical picture may sometimes simulate the hypo-pigmented plaques of tuberculoid leprosy and the diagnosis can be settled by laboratory finding of the causative bacteria. The neurological signs show anesthesia of the hypopigmented patches of tuberculoid leprosy. Pityriasis rosea - the herald patch, the distinct distribution of the eruption along the line of the ribs and the negative microscopic examination for any fungal element will help in the differential diagnosis. Erythrasma - the two conditions may co-exit together. Diagnosis can be confirmed by microscopic detection of the causative organism and the pink fluorescence with Wood‘s Light in erythrasma. Seborrheic dermatitis - the condition is more inflammatory and the sites involved are localized to certain areas as the intertriginous. The greasy scales covers lesions of seborrheic dermatitis. Secondary stage of syphilis - the history, the clinical features, the color of the lesions and positive serological tests of syphilis confirm the differential diagnosis. Treatment Preventive measures: are very important to prevent re-infection.
Certain expensive clothes can be washed the ordinary way by adding Nizoral shampoos to hot water and soak the clothes for one hour, then wash and rinse. Towels and bed sheets should be also boiled and ironed to destroy the fungus.
Active treatment Selenium sulfide 2.5 per cent (Selsun shampoo) applied every other day for two weeks clear most of the lesions. Take care of the genitalia and eyes due to the possibility of local irritations. Topical azoles such as Ecanozole (Pevaryl spray) and other anti- fungal preparations are also effective, but are more expensive. Spray or shampoo preparations are easier to use than creams or ointments. Once or twice daily application of the medication is usually required for several weeks. Topical Corticosteroids, which may improve the condition temporary, are not recommended. Treatment of Recurrent Cases Most failures of topical therapy are either due to inaccurate diagnosis, inadequate treatment, missing out some lesions or re-infection either auto-infection or from other sources. Treatment with one percent Ecanozole citrate spray (Pevaryl) is effective and easy to be used especially on widespread areas. Oral Itraconazole used in a single dose of 400 mg and ketoconazole total adult dose 800-1000 is very effective. Children are given smaller doses depending on their weight. The value of oral treatment with 400 mg. of Fluconazole (adult dose) in a single dose proved to be effective in the treatment of pityriasis versicolor. These medications are expensive and some patients can not afford the cost. Oral azoles are better kept as a reserve for reluctant or recurrent cases of T. versicolor. Oral antifungal medications are not usually recommended as a routine in T. Versicolor where the lesion may clear with topical preparations such as Ecanozole cream, spray and shampoo alone. In recurrent cases, treatment may take a longer time and it is better to use topical Ecanozole (Pevaryl sachets). One sachet can be used to rub the skin twice weekly for one month and later once weekly for three months or for longer periods Care and precautions to prevent auto or re-infection from contacts.
PIEDRA This is a fungal infection confined to the hair shafts and resulting in the formation of superficial nodules on the infected hair. Young girls are frequently affected. Familial outbreaks may occur. Clinical features There are two varieties of Piedra, the black and the white (asteroid), which are caused by Piedra hortae and Trichosporon beigelii, respectively. Black Piedra is characterized by the presence of firmly adherent black, hard, gritty nodules, which are composed of a mass of fungus cells on the hair shaft, which causes its disintegration , britling and breaking. These nodules vary in size from microscopic to 1 mm or more in diameter. This type occurs in tropical countries and affects monkeys as well as man. White Piedr Systemic infections due to Trichosporon may affect many different sites including the liver, spleen and heart. Occasionally deep dermal nodules may occur. Diagnosis Smear: Microscopically hyphae, arthrospores and budding cells are present. Culture: In culture, the fungus has slow growth, dark and compact, and usually heaped at the center. In cultures of T. beigelii the colonies develop rapidly and are creamy and wrinkled, later becoming deeply furrowed and folded. Treatment The organisms of White Piedra are surprisingly resistant in vitro to the Azole antifungal drugs. Shaving or cutting the hair is an effective method of treatment. To prevent recurrence, antifungal preparations such as Benzoic Acid Compound Ointment BPC or a 1:2000 solution of mercury perchloride may be applied to the scalp after shampooing.
|
||||||||||||||||||||||
| Contents | << Previous Chapter | Next Chapter >> | Search |